Artikel
Ganz gleich, ob Sie pflegende, medizinische oder ärztliche Fachperson oder völlig neu in der Kontinenzversorgung sind, Wellspect Education bietet Lerninhalte für Ihren Kenntnisstand.
Ganz gleich, ob Sie pflegende, medizinische oder ärztliche Fachperson oder völlig neu in der Kontinenzversorgung sind, Wellspect Education bietet Lerninhalte für Ihren Kenntnisstand.

key:global.content-type: Artikel
Sichten Sie die klinischen Evidenz, die für die verbesserten Ergebnisse der Anwendung von TAI bei pädiatrischen Patienten spricht, wenn sie mit einem individuellen Ansatz zu Beginn der TAI gekoppelt sind.

key:global.content-type: Artikel
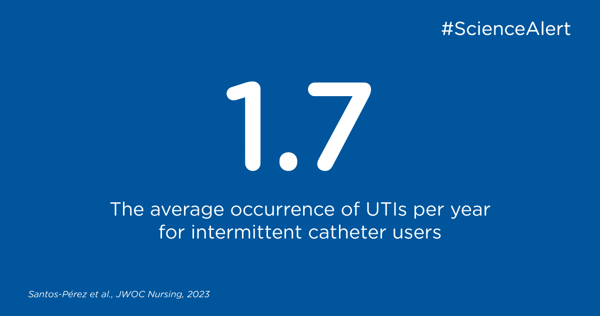
Diese Studie bietet wertvolle Einblicke in die Erfahrungen von Personen, die den IK durchführen, um die Patientenversorgung und -unterstützung zu optimieren.
key:global.content-type: Artikel
Der Einfluss der transanalen Irrigation auf die Darmmikrobiota könnte sich positiv auf das Immunsystem auswirken und zu einer Verringerung von Harnwegsinfektionen beitragen, wie aus dieser klinischen Studie von Futura et. al.

key:global.content-type: Artikel
Klinische Daten zur transanalen Irrigation als Mittel zur Behandlung des neurogenen Darms in der pädiatrischen Population mit Spina bifida

key:global.content-type: Artikel
In diesem Artikel fassen wir die wichtigsten Ergebnisse und Empfehlungen einer Studie von Bauer et al. aus dem Jahr 2023 zusammen, die die intermittierende Katheterisierung (IK) bei Kindern und Jugendlichen im schulischen Umfeld untersucht.

key:global.content-type: Publication highlight
Die traditionelle Sichtweise der Sterilität des Urins wurde durch die Entdeckung des Harnmikrobioms, d. h. einer Mischung aus Bakterien und Mikroorganismen in den Harnwegen, in Frage gestellt. Diese einzigartige Beziehung zwischen Mikroben und Menschen ist noch nicht vollständig verstanden, hat aber in den letzten zehn Jahren in der klinischen Forschung viel Aufmerksamkeit erregt.

key:global.content-type: Artikel
In diesem Publikations-Highlight können Sie über eine Studie über chronische idiopathische Verstopfung bei Kindern lesen und darüber, wie eine Darmspülung, auch transanale Irrigation (TAI) genannt, die Selbstständigkeit verbessern und die Symptome reduzieren kann.

key:global.content-type: Artikel
Eine Harnröhrenstriktur ist eine krankhafte Verengung der Harnröhre und wird häufig durch ein Trauma oder eine Entzündung verursacht. Da die Katheterisierung eine Ursache für Strikturen ist, sind die nicht-traumatische Katheterisierungstechnik und das Kathetermaterial wesentliche Bestandteile, um das Auftreten dieser Komplikationen zu verhindern.

key:global.content-type: Artikel
In mehr als 40 Jahren auf dem Markt wurde LoFric auf verschiedene Weise eingesetzt und dokumentiert. Neben der effizienten Entleerung der Blase umfasst der vielseitige Einsatz von LoFric die Behandlung und Vorbeugung von wiederkehrenden Strikturen, die Verabreichung einer Chemotherapie durch Instillation der Blase und die Lösung seltener Komplikationen.

key:global.content-type: Publication highlight
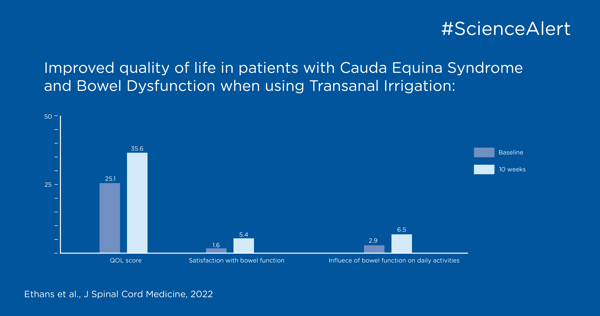
In diesem Publikations-Highlight können Sie nachlesen, wie Sie Darmfunktionsstörungen bei Personen mit Cauda-equina-Syndrom behandeln können.
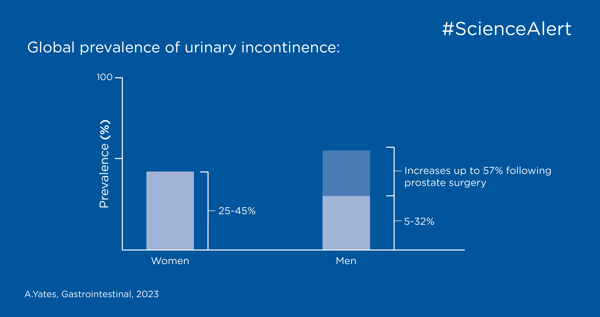
In diesem Publikations-Highlight können Sie über die Erkennung, Beurteilung und Behandlung von Harninkontinenz und Darmkontrollproblemen lesen.
Es kann überwältigend sein, auf dem Laufenden zu bleiben und den Wahrheitsgehalt von wissenschaftlichen Artikeln und klinischen Studien zu bestimmen, daher haben wir eine Checkliste zusammengestellt, die Ihnen helfen kann.
